Podiatry Services for Fort Walton Beach and Niceville FL
Many podiatric conditions can be treated in our office under the care of our Podiatrist Paul J. Kalin, DPM and our exceptional staff. In some cases, surgery will be performed at a hospital. Foot conditions involving damage to underlying tissues are best treated with surgery. Conditions involving a change in the conformation of the foot or toes are also amenable to correction with surgery. Podiatrists are specially trained in the use of a variety of surgical techniques to address these problems, to minimize pain and to prevent the loss of function of any part of the foot. Podiatrists are also familiar with all available treatment options to determine when surgery is necessary, and when it can be avoided.

Bunions
Bunions are one of the most common foot disorders treated by Dr. Kalin. In fact, bunions are one of the most common disorders treated by most podiatrists across the country. More than half the women in America have bunions, a common deformity often blamed on wearing tight, narrow shoes. Bunions cause the base of your big toe (Metatarsophalangeal Joint) to enlarge and protrude.
The skin over it may be red and tender. This can be acquired through time or it can be congenital (you got it from your family).
Wearing any type of shoe may be painful when you have a bunion. The joint involved flexes with every step you take. The bigger your bunion gets, the more it hurts to walk. Bursitis (inflammation) may also set in. Your big toe may angle towards your second toe, or even move all the way under or over it. The skin on the bottom of your foot may also become thicker and painful.
Pressure from your big toe may force your second toe out of alignment, sometimes causing it to overlap your third toe. If your bunion gets too severe, it may cause difficulty in walking. Your pain may become chronic and you may develop arthritis.
Most bunions can be treated conservatively with wider & softer shoes, pads to relieve the pressure and/or medications. If this does not help then surgical treatment is indicated.
Bunion Surgery:
Bunion surgery, or bunionectomy, realigns the bone, ligaments, tendons and nerves so your big toe can be brought back to its correct position and the bump on the inside of the joint removed. Many bunion surgeries are performed on a same-day basis (no hospital stays) using a local anesthesia. During your recovery it is common to have pain and swelling. This swelling and stiffness may be persistent for several months.
A bunion occurs when the joint at the base of your big toe becomes enlarged, sore and swollen. Your big toe may start to angle toward your second toe, or move underneath it. Women are most affected by bunions, which are often caused by wearing narrow, tight shoes, or high heels. A bunionette occurs on the other side of the foot, near your small toe, and is much smaller than a bunion.
Diagnosis:
A podiatrist can usually diagnose a bunion during a physical exam. An X-ray may provide further information about the joint, the angle of the toe, and if arthritis or gout are concerns to further investigate.
Treatment:
Wearing comfortable shoes with a wide toe-box at the first signs of a bunion appearing can decrease its growth and reduce any further complications. Resting the foot, using anti-inflammatory medications and icing the area may help. In some cases a cortisone shot at the base of the big toe may help. In cases when the bunion is causing severe pain, surgery may be performed to remove the bony bump and to realign the toe.
Without Treatment:
Ignoring a bunion will lead to increased pain and the chance of contracting bursitis, when the small fluid-filled sac next to the joint becomes inflamed. Depending on how severe your bunion is, your foot can become deformed and continue to cause chronic pain.

Calluses and Corns
What are Foot Corns & Calluses?
A callus is an area of hard, thickened skin that can occur across the ball of the foot, on the heel, or on the outer side of the big toe. While many consider them a skin problem, they actually are systemic of a problem with the bone.
Calluses have painful nerves and bursal sacs (fluid-filled balloons that act as shock absorbers) beneath them, causing symptoms ranging from sharp, shooting pain to dull, aching soreness.
Calluses form from repeated friction and pressure, as the shoe (or ground) rubs against a bony prominence (bone spur) on the toe or foot. The skin thickens in response to this pressure. Small amounts of friction or pressure over long periods of time cause a corn or callus. A great deal of friction or pressure over shorter periods of time can cause blisters or open sores. Calluses typically develop under a metatarsal head (the long bone that forms the ball of the foot) that is carrying more than its fair share of the body weight, usually due to it being dropped down or due to its longer length.
Calluses can be treated with over-the-counter callus removers that have strong acids that peel this excess skin away after repeated application. You should be careful with these products as they can cause chemical burns when not used correctly. Begin by soaking your feet in warm soapy water and gently rubbing away any dead skin that loosens. A pumice stone or emery board is then used to “file” this thickened skin. Apply a good moisturizer to the hardened areas to keep them softer and relieve pain. Non-medicated corn pads or moleskin (a thin fuzzy sheet of fabric with an adhesive back) can relieve calluses, but should be removed carefully to avoid tearing the skin.
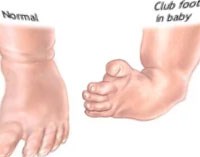
Club Foot
Clubfoot is one of the most common non-life threatening major birth defects. It affects your child’s foot and ankle, twisting the heel and toes inward. It may look like the top of the foot is on the bottom. The clubfoot, calf and leg are smaller and shorter than normal. Clubfoot is not painful, is correctable, and your baby is probably otherwise normal.
Approximately one in every 1,000 newborns has clubfoot. Of those, one in three have both feet clubbed. The exact cause is unknown. Two out of three clubfoot babies are boys. Clubfoot is twice as likely if you, your spouse or your other children also have it. Less severe infant foot problems are common and are often misdiagnosed as clubfoot.
The goal of treating clubfoot is to make your newborn’s clubfoot (or feet) functional, painless and stable by the time he or she is ready to walk. Doctors start by gently stretching your child’s clubfoot toward the correct position. They put on a cast to hold it in place. One week later, they take off the cast and stretch your baby’s foot a little more, always working it toward the correct position. They apply a new cast, and one week later you come back and do it again.
This process (called serial casting) slowly moves the bones in the clubfoot into proper alignment. Doctors use X-rays to check the progress. Casting generally repeats for 6-12 weeks, and may take up to four months. About half the time, your child’s clubfoot straightens with casting. If it does, he or she will be fitted with special shoes or braces to keep the foot straight once corrected. These holding devices are usually needed until your child has been walking for up to a year or more.
Muscles often try to return to the clubfoot position. This is common when your child is 2-3 years old, but may continue up to age 7. Sometimes stretching, casting and bracing is not enough to correct your baby’s clubfoot. He or she may need surgery to adjust the tendons, ligaments and joints in the foot/ankle.
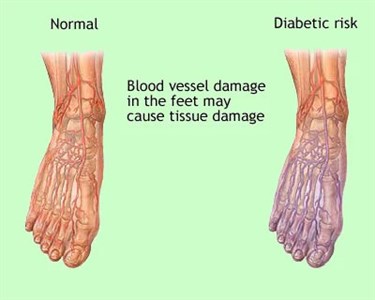
Diabetic Foot Care
Why Is Diabetic Foot Care Important?
According to the American Diabetes Association, about 15.7 million people (5.9 percent of the United States population) have diabetes. Nervous system damage (also called neuropathy) affects about 60 to 70 percent of people with diabetes and is a major complication that may cause diabetics to lose feeling in their feet or hands. Foot problems are a big risk in diabetics. Diabetics must constantly monitor their feet or face severe consequences, including amputation. With a diabetic foot, a wound as small as a blister from wearing a shoe that’s too tight can cause damage. Diabetes decreases blood flow, so injuries are slow to heal. When your wound is not healing, it’s at risk for infection. As a diabetic, your infections spread quickly. If you have diabetes, you should inspect your feet every day. Look for puncture wounds, bruises, pressure areas, redness, warmth, blisters, ulcers, scratches, cuts and nail problems.
Here’s some basic advice for taking care of your feet:
- Always keep your feet warm.
- Don’t get your feet wet in snow or rain.
- Don’t put your feet on radiators or in front of the fireplace.
- Don’t smoke or sit cross-legged. Both decrease blood supply to your feet.
- Don’t soak your feet.
- Don’t use antiseptic solutions, drugstore medications, heating pads or sharp instruments on your feet.
- Trim your toenails straight across. Avoid cutting the corners. Use a nail file or emery board. If you find an ingrown toenail, contact our office.
- Use quality lotion to keep the skin of your feet soft and moist, but don’t put any lotion between your toes.
- Wash your feet every day with mild soap and warm water.
- Wear loose socks to bed.
- Wear warm socks and shoes in winter.
- When drying your feet, pat each foot with a towel and be careful between your toes.
- Buy shoes that are comfortable without a “breaking in” period. Check how your shoe fits in width, length, back, bottom of heel, and sole. Avoid pointed-toe styles and high heels. Try to get shoes made with leather upper material and deep toe boxes. Wear new shoes for only two hours or less at a time. Don’t wear the same pair everyday. Inspect the inside of each shoe before putting it on.
- Don’t lace your shoes too tightly or loosely.
- Choose socks and stockings carefully. Wear clean, dry socks every day. Avoid socks with holes or wrinkles. Thin cotton socks are more absorbent for summer wear. Square-toes socks will not squeeze your toes.
When your feet become numb, they are at risk for becoming deformed. One way this happens is through ulcers. Open sores may become infected. Another way is the bone condition Charcot (pronounced “sharko”) foot. This is one of the most serious foot problems you can face. It warps the shape of your foot when your bones fracture and disintegrate, and yet you continue to walk on it because it doesn’t hurt. Diabetic foot ulcers and early phases of Charcot fractures can be treated with a total contact cast.
The shape of your foot molds the cast. It lets your ulcer heal by distributing weight and relieving pressure. If you have Charcot foot, the cast controls your foot’s movement and supports its contours if you don’t put any weight on it. To use a total contact cast, you need good blood flow in your foot. The cast is changed every week or two until your foot heals. A custom-walking boot is another way to treat your Charcot foot. It supports the foot until all the swelling goes down, which can take as long as a year. You should keep from putting your weight on the Charcot foot. Surgery is considered if your deformity is too severe for a brace or shoe.
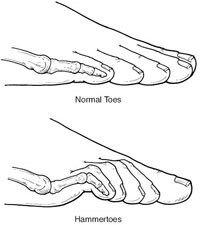
Hammer Toe
A Hammertoe is a deformity of the second, third or fourth toes. In this condition, the toe is bent at the middle joint, resembling a hammer. Left untreated, hammertoes can become inflexible and require surgery. People with hammertoes may have corns or calluses on the top of the middle joint of the toe or on the tip of the toe. They may also feel pain in their toes or feet and have difficulty finding comfortable shoes.
Causes of hammertoe include improperly fitting shoes and muscle imbalance. Treatment for the condition typically involves shoes with soft, roomy toe boxes and toe exercises to stretch and strengthen the muscles. Commercially available straps, cushions or non-medicated corn pads may also relieve symptoms.
Diagnosis:
A physical exam will confirm the presence of a hammer toe. An X-ray can show more about the patient’s specific condition.
Treatment:
Treating a hammer toe before it becomes “fixed” in position is essential. Orthotics, splints, or wearing shoes with roomy toe-boxes may help non-severe cases of hammer toe. In severe cases, surgery may be performed.
Without Treatment:
Pain and walking difficulty may increase, and a permanent deformity may occur. Repeated friction to the tip or the top of the toe can lead to wounds and infection.
Heel Pain
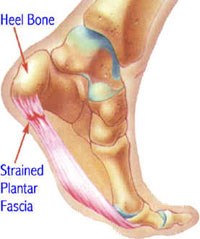
What causes Heel Pain & Plantar Fasciitis?
Heel pain is one of the leading causes that patients visit Toes Are Us to have treated. Plantar fasciitis (or heel pain) is commonly traced to an inflammation on the bottom of the foot. Dr. Kalin can evaluate your arch pain, and may prescribe customized shoe inserts called orthotics to help alleviate the pain you are experiencing.
Plantar fasciitis is caused by inflammation of the connective tissue that stretches from the base of the toes, across the arch of the foot, to the point at which it inserts into the heel bone. Also called “heel spur syndrome,” the condition can usually be successfully treated with conservative measures such as use of anti-inflammatory medications and ice packs, stretching exercises, orthotic devices, and physical therapy.
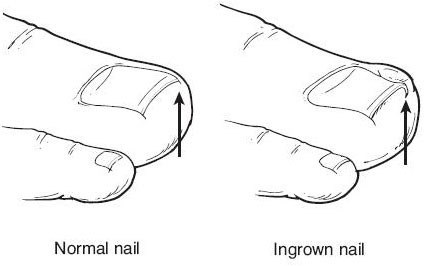
Ingrown Toenails
What is an Ingrown Toenail?
Ingrown toenails often are the result of trimming your toenails too short, particularly on the sides of your big toes.
While they are very common, ingrown toenails can also be very painful. When trimming your nails, avoid tapering the corners so that the nail curves with the shape of your toe. The sides of the nail will curl down and dig into your skin. Shoes that are too tight or short also may cause ingrown toenails. Ingrown toenails start out hard, swollen and tender, and later, may become sore, red and infected. Your skin may start to grow over the ingrown toenail.
Soaking your foot in warm, soapy water several times each day is usually a good way to treat an ingrown nail. We recommend that you visit our office and let Dr. DOCTOR determine the best course of treatment for your condition.
Antibiotics are sometimes prescribed if an infection is present. Part of your ingrown toenail (partial nail plate avulsion) may need to be surgically removed if an acute infection occurs. The procedure involves injecting the toe with an anesthetic and cutting out the ingrown part of the toenail.
You can prevent ingrown toenails by:
- Trimming your toenails straight across with no rounded corners.
- Ensuring that your shoes and socks are not too tight.
- Keeping your feet clean at all times.
An ingrown toenail (also known as onychocryptosis) occurs when the nail grows sideways into the toe, and not outward. The result is pain in the side of the toe. The big toe is most commonly affected. It can be caused by any situation that interferes with the proper outward growth of the nail, such as improper trimming of the nail or incorrect footwear.
Diagnosis:
The diagnosis of an ingrown toenail can be made on the basis of the appearance of the toe. A history is also obtained to determine the cause of the ingrown toenail, and to address any predisposing conditions.
Treatment:
In some cases, the edge of the nail can be separated from the side of the toe. Padding is the placed between the nail and the toe to encourage growth in the correct direction. Many cases require surgical removal of the toenail. A new, normal nail then grows in over the next several months.
Without Treatment:
The nail may continue to grow into the side of the toe. This can lead to progressive pain or recurring infection. It is most serious in people with underlying medical problems such as diabetes or peripheral vascular disease.
Sports Injuries
Podiatrists & Sports-Related Injuries:
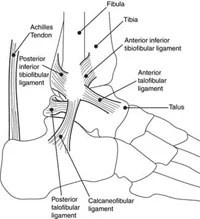
Whether you are a professional athlete or play sports just for fun, the demands made on your feet and lower limbs can lead to a range of injuries, including blisters, sprained ankles, torn ligaments, shin splints (leg pain), knee pain, low back pain and other joint or muscle problems. Added to these are common complaints such as corns, calluses and Athlete’s foot. Your running style, poor footwear and even minor limb length differences can also contribute to sports injury.
Visiting a podiatrist like Dr. Paul Kalin should be your fist step towards getting back on your feet after a sports injury. Dr. Kalin can not only help treat your current foot or ankle pain, but provide you with helpful tips to prevent future sports injuries.
Here are some tips for athletic foot care:
- Wash your feet every day, and dry thoroughly.
- Wear only good-quality, well-fitting cotton socks.
- Always use the correct shoe for each sport and surface.
- Get in shape. Being overweight or out of shape places added stress on the feet. Condition yourself gradually with stretching exercises for 15-20 minutes before starting and after any activity (“warm-up” and “warm-down”).
- Wear correct shoes. Footwear should be given the same consideration as any other piece of sporting equipment. Sports shoes should protect as much as possible, be durable, and should be right for the sport and surface. If running, the shoe should have adequate cushioning in the mid-sole and a flared heel for stability.

Nail Fungal Infection
Do You Have Toenail Fungus?
Many people don’t realize they have a fungal nail problem. Moreover, many people that do never seek treatment. Still, fungal toenail infections are a common foot health problem.
Fungal toenail infections can persist for years without ever causing pain. The disease, characterized by a change in a toenail’s color, is often considered nothing more than a mere blemish, but it can present serious problems if left untreated.
Also referred to as Onychomycosis, fungal nail infections are an infection underneath the surface of the nail, which can also penetrate the nail. In addition to causing difficulty and pain when walking or running, fungal nail infections are often accompanied by a secondary bacterial and/or yeast infection in or about the nail plate.
A group of fungi called dermatophytes easily attack the nail, thriving off keratin, the nail’s protein substance. When the tiny organisms take hold, the nail may become thicker, yellowish-brown or darker in color, and foul smelling. Debris may collect beneath the nail plate, white marks frequently appear on the nail plate, and the infection is capable of spreading to other toenails, the skin, or even the fingernails. Nail bed injuries may make the nail more susceptible to all types of infection, including fungal infection. Those who suffer chronic diseases, such as diabetes, circulatory problems, or immune-deficiency conditions, are especially prone to fungal nails. Other contributory factors may be a history of Athlete’s foot and excessive perspiration.
You can prevent fungal nail infections by taking these simple precautions:
- Exercise proper hygiene and regularly inspect your feet and toes
- Keep your feet clean and dry.
- Wear shower shoes in public facilities whenever possible.
- Clip your nails straight across so that the nail does not extend beyond the tip of the toe.
- Use a quality foot powder – talcum, not cornstarch – in conjunction with shoes that fit well and are made of materials that breathe.
- Avoid wearing excessively tight hosiery, which promotes moisture. Socks made of synthetic fiber tend to “wick” away moisture faster than cotton or wool socks, especially for those with more active life styles.
- Disinfect home pedicure tools and don’t apply polish to nails suspected of infection.
Depending on the type of infection you have, over-the-counter liquid antifungal agents, while sometimes effective, may not prevent a fungal infection from recurring. A topical or oral medication may need to be prescribed, and the diseased nail matter and debris removed by a process called debridement.
In some cases, surgical treatment is prescribed, during which the infected fungal nail is removed. Permanent removal of a chronically painful nail, which has not responded to any other treatment, permits the fungal infection to be cured, and prevents the return of a deformed nail.
Nail Fungal Laser Treatment
What is toenail fungus?
Nail fungus, or onychomycosis, is an ailment that plagues 10% of the world’s population. Onychomycosis causes toenails to become yellow or discolored and if not treated, will cause them to become brittle and thick and separate from the nail bed over time.
What does laser treatment do?
Light from the laser filters through the nail and the adjacent tissue. Pigment in the fungi absorbs the light, heating it and harming the organism. The elimination of fungus will allow your nail to grow normally.
What results can I expect?
During clinical research, 68% of patients exhibited post-treatment improvement in the percent of nail with no infection. The extent of progress you will experience is reliant on individual circumstances and is something your doctor will discuss with you.
What is the treatment like?
During laser nail fungus treatment, the laser is passed over the infected nails and bordering skin. This process will be repeated several times by your physician until a sufficient amount of energy has extended into the nail bed. During this treatment, you may feel your nail grow warmer.
Treatment Duration:
One treatment lasts about 20 minutes and can treat 5-10 nails. Be sure to check with your doctor as duration times vary.
Number of Treatments:
Typically, patients demonstrate improvement after just one treatment. This number varies, however, depending on the severity of the infection.
Before the Procedure:
Please remove all nail polish and decorations the day before the procedure.
During the procedure:
Patients report that the process is generally comfortable. You may feel a small hot pinch near the end, lasting momentarily.
After the Procedure:
Your nail might feel warmer than normal for a few minutes following the procedure. Most patients are able to resume normal activities immediately.
Long Term:
A successful treatment will result in a new and healthier nail growing. As nails tend to grow slowly, it may take up to a year for results to be complete.
Can the fungal infection return?
While your nail will show signs of immediate improvement following the fungus nail treatment, it is important to continue with home care techniques to dissuade recurrence. Re-infection is possible as the fungus is located almost everywhere in the environment.
Service Policy
Please call (850)863-1238
